Our work
Our belief in the power of design to improve people’s lives is reflected in how we approach our work. It is an approach that is collaborative and continuous, because places are constantly changing and evolving.
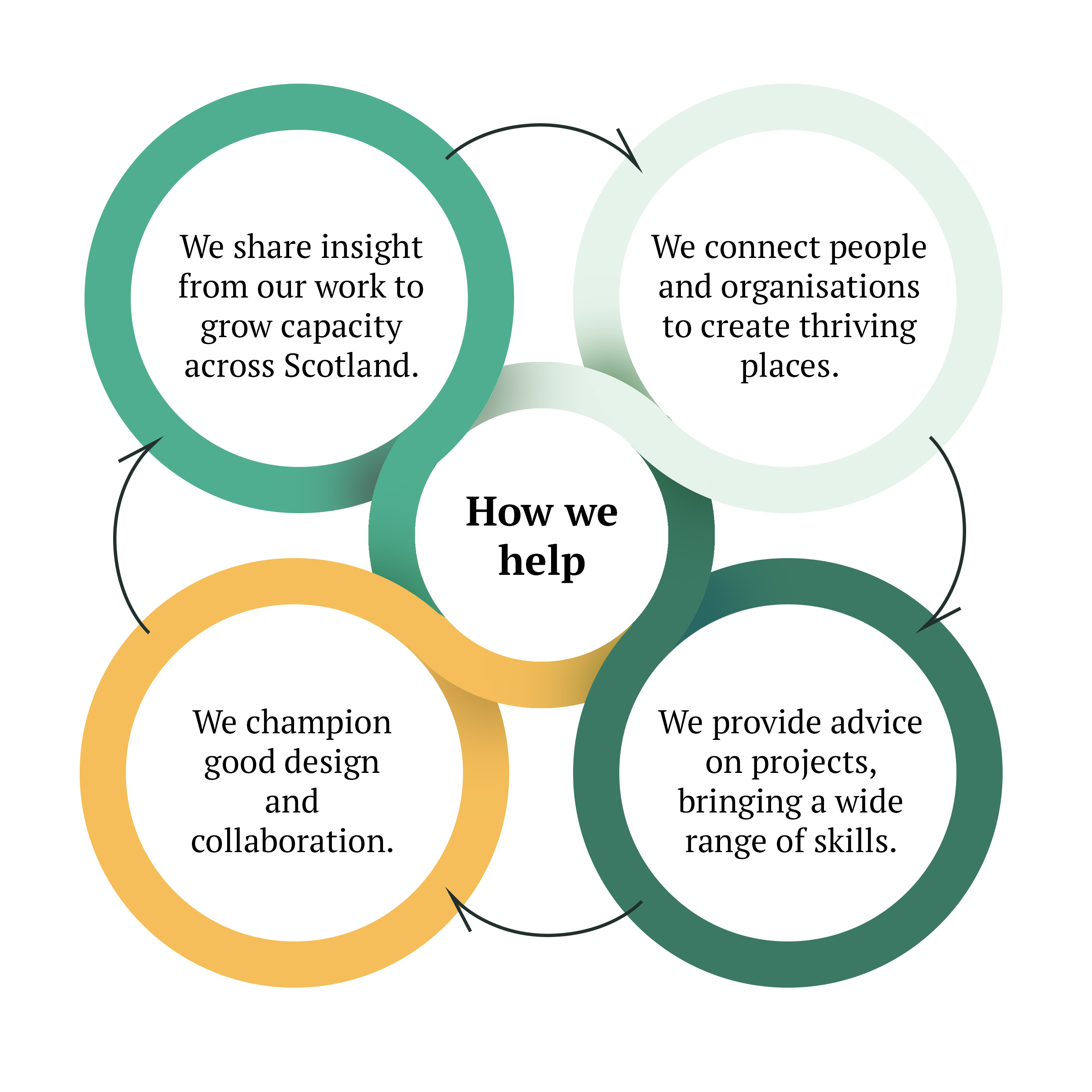
We want the Place Principle to be the normal way of doing things in Scotland. How we help make that happen is by promoting good design and collaboration, connecting people and organisations, providing advice and skills, and sharing insights from our work.
If you would like to explore how we can help, please get in touch with us.
Our approach
The diagram (right) illustrates how we help. Click on the links below to navigate to the selected sections:
We share insight from our work to grow capacity across Scotland
We connect people and organisations to create thriving places
We provide advice on projects, bringing a wide range of skills

Example: Collaborating to create learning spaces
The spaces we work and learn in play a huge part in shaping our mental health, happiness, and ability to learn. How can the room we work in make a lesson better or more inspiring? Our Shared Learning toolkit will help guide you and your pupils step-by-step on a collaborative mission to find the answers.
We connect people and organisations to create thriving places
The outcomes are always so much better for everyone involved when we all sit down and discuss our needs and concerns together. That is why we connect people and organisations to share their experiences. We have developed a series of events called the Place Forum where we explore current issues and practice. In our work on the climate emergency, we are working with communities to take place-based action on climate.
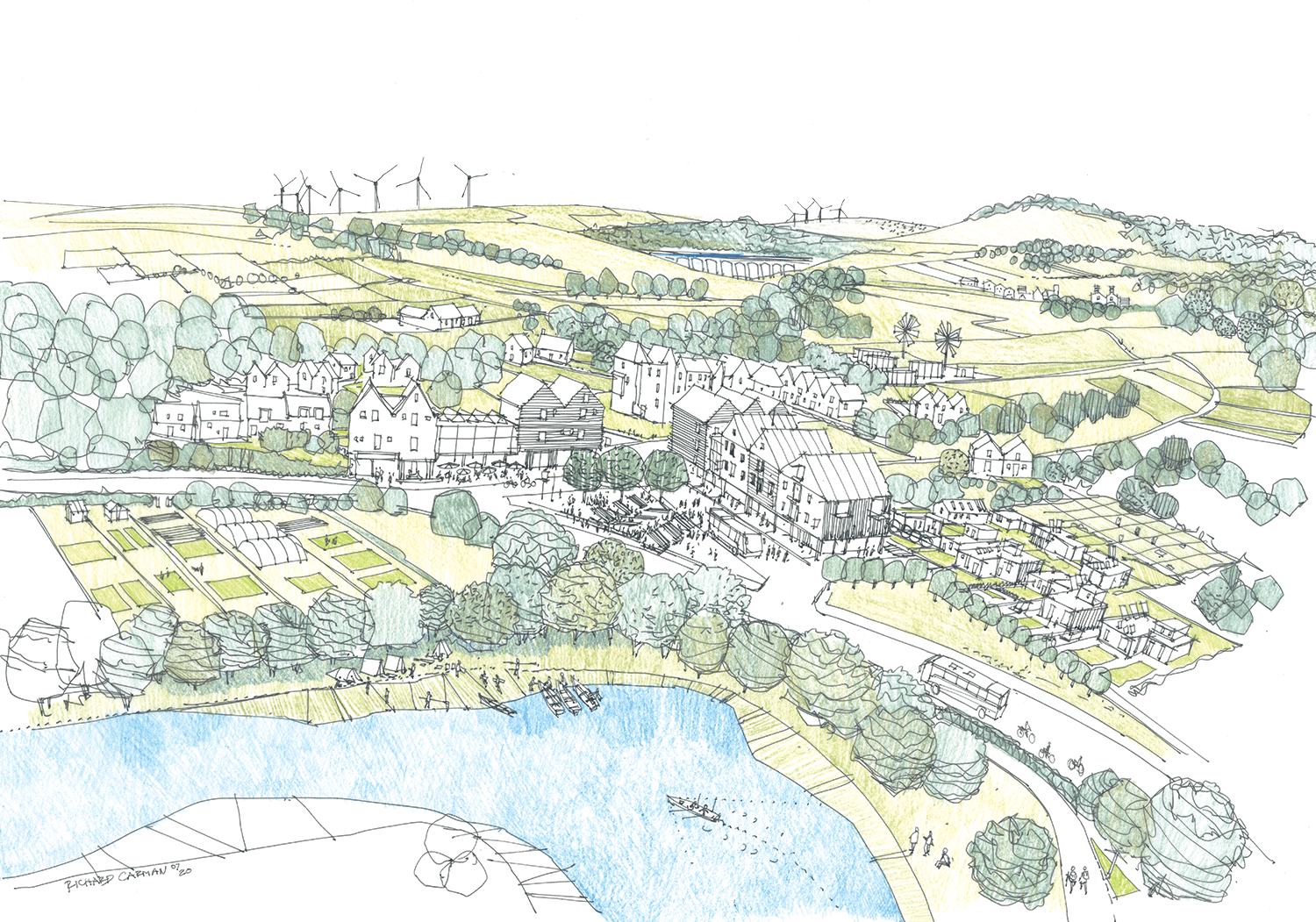
Example: Tackling climate change together
To protect Scotland from the impacts of climate change, we all need to work together to adapt the ways we live, work, play and move in our cities, towns and villages. We are working with local communities to support place-based climate action in a network of small Scottish towns.
Image credit: Richard Carman
We provide advice on projects, bringing a wide range of skills
No matter where you are on your journey, we can bring a wealth of expertise and experience to help you at every stage, or just whenever you need us.
We provide expert advice on Scotland’s learning estate and our healthcare buildings, as well as how to work together to create thriving places. We take a leading role on place in the Key Agencies Group, ensuring that the Place Principle is becoming a reality.

Example: Taking a whole-place collaborative approach
We have recently worked on several projects that have contributed to the whole-place collaborative approach to the regeneration of Alva. These include the planning of carbon conscious places, meeting the needs of an ageing population through a caring place and addressing the regeneration of Alva’s town centre.
Image credit: 3DReid
We champion good design and collaboration
Understanding why good design is important and the difference it can make to people and communities is one of the core messages we share. We champion examples of people working together to design our places.
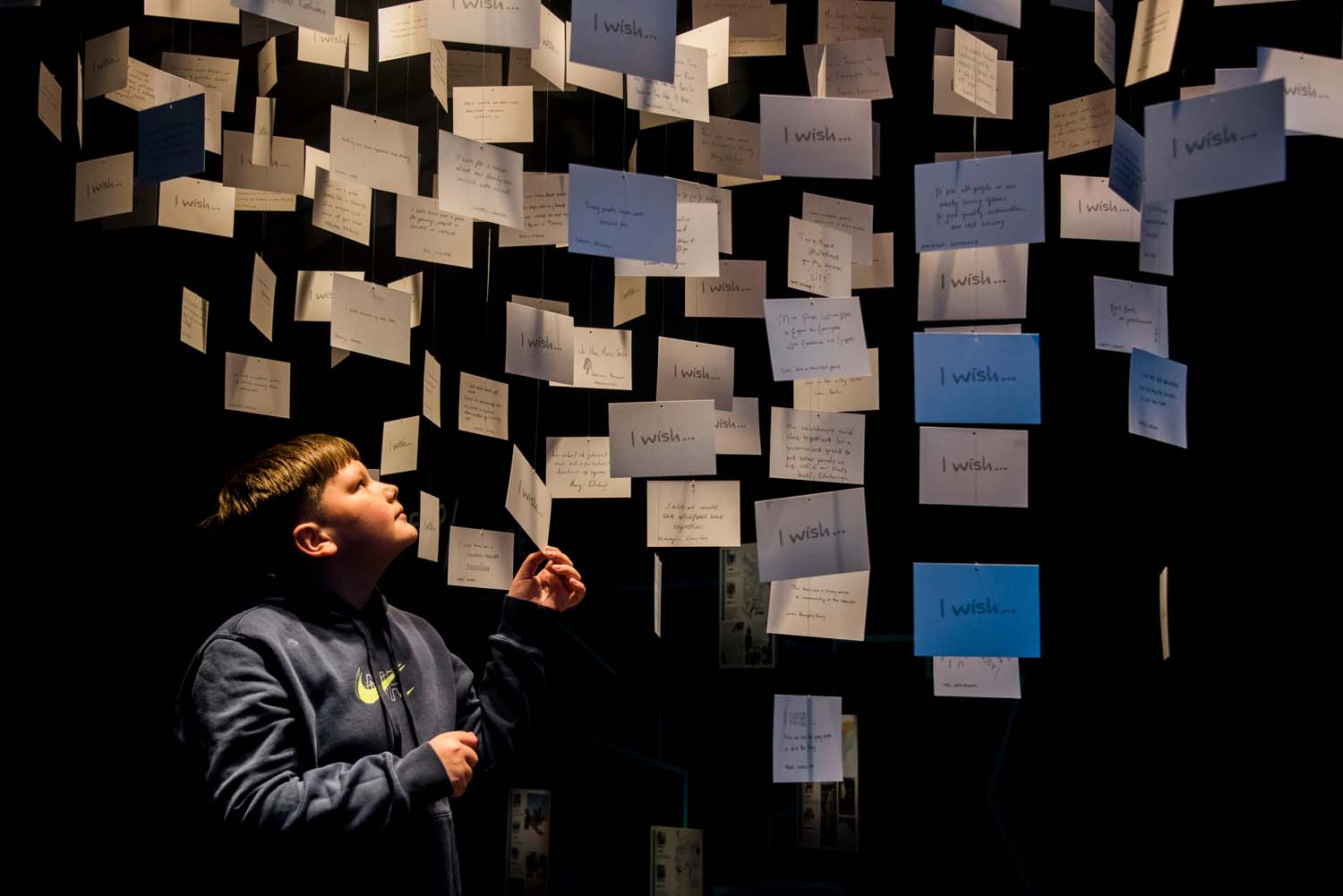
Example: Connecting citizens and designers
An exhibition at V&A Dundee in 2021 showed just what can happen when designers and residents come together to plan a better future for the places they call home. What if...?/Scotland, created by 7N Architects and promoted by the Scotland + Venice partnership, demonstrated the power of design.
Image credit: Alan Richardson
Helpful tools and resources
We have plenty of useful and inspiring documents and videos to help you get started or keep going.
Our latest news, blogs and events

A new home for Architecture and Design Scotland

Learning from the Climate Action Towns at the Gathering event and resource launch

The Recap: a weekly update from Architecture and Design Scotland

The Recap: a weekly update from Architecture and Design Scotland

Key trends that mean we need to use our town centres differently - event

Roadshow series highlights huge potential for communities across the country
Header image credit: Miss Lydia Photography
Get in touch
If you have a question or would like to find out more about the work we do and how we can help you, please get in touch.

